Fatty Liver Disease: An Overview | Alfa Gastro and Liver Care, Ahmedabad

Fatty liver disease refers to a condition where excess fat accumulates in the liver cells. While the liver normally contains a small amount of fat, an overabundance can interfere with its normal functioning. Over time, if left untreated, fatty liver disease can lead to more serious liver conditions, including cirrhosis, liver failure, or even liver cancer. There are two main types of fatty liver disease: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). Both types share similar symptoms and causes but differ in their triggers.
What is Fatty Liver Disease?
Fatty liver disease occurs when fat builds up in liver cells, causing inflammation and scarring. Although the liver is resilient and can often repair itself, when fatty deposits persist and the liver becomes overwhelmed, the damage can become permanent.
This condition is commonly seen in individuals who have obesity, h
igh cholesterol, diabetes, or consume excessive alcohol.
The liver is essential for processing toxins, producing bile for digestion, and storing energy in the form of glycogen. When fat accumulates in the liver, its ability to perform these functions efficiently diminishes. In the early stages, fatty liver may present with few or no symptoms. However, as the disease progresses, it can lead to significant complications.
Types of Fatty Liver Disease
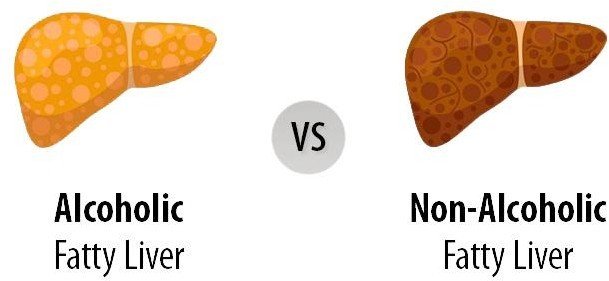
- Non-Alcoholic Fatty Liver Disease (NAFLD): This is the most common form of fatty liver disease and occurs in people who consume little or no It is often linked to obesity, type 2 diabetes, high cholesterol, and other metabolic conditions. NAFLD can range from simple fatty liver (steatosis) to a more severe form known as non-alcoholic steatohepatitis (NASH), where inflammation and liver damage are present.
- Alcoholic Fatty Liver Disease (AFLD): This type is caused by excessive alcohol consumption. Alcohol can cause fat to accumulate in liver cells, leading to inflammation and liver damage. The severity of AFLD depends on the amount and duration of alcohol intake.
Symptoms of Fatty Liver Disease
Fatty liver disease is often asymptomatic in the early stages, making it difficult to diagnose without testing. However, as the disease progresses, individuals may experience:
- Fatigue or feeling constantly tired
- Discomfort or pain in the upper right side of the abdomen
- Unexplained weight loss
- Enlarged liver (hepatomegaly), which may be detected by a doctor during a physical exam
- Jaundice, which is a yellowing of the skin and eyes (in more severe cases)
- Swelling in the abdomen or legs due to fluid retention
- Nausea or loss of appetite
- Confusion or difficulty concentrating, especially if liver function is significantly impaired
As the condition progresses to more severe forms like NASH or cirrhosis, these symptoms may become more pronounced.
Causes of Fatty Liver Disease
The causes of fatty liver disease are varied and can depend on the type of fatty liver:
1. Non-Alcoholic Fatty Liver Disease (NAFLD):
- Obesity: Excess body weight, especially abdominal fat, is a major risk factor for fatty liver disease.

- Type 2 Diabetes: Insulin resistance and high blood sugar levels can lead to fat accumulation in the liver.

- High Cholesterol and Triglycerides: Elevated levels of fat in the blood can contribute to fatty liver.

- Metabolic Syndrome: A combination of high blood pressure, obesity, and insulin resistance increases the risk.

- Genetics: Family history and genetic factors can predispose individuals to fatty liver disease.

- Poor Diet: Diets high in fats, sugars, and refined carbohydrates contribute to fatty liver development.
2. Alcoholic Fatty Liver Disease (AFLD):
- Excessive Alcohol Consumption: The liver processes alcohol, and excessive drinking over time can cause fat to accumulate and inflammation to develop, eventually leading to liver damage.
Progression of Fatty Liver Disease
Fatty liver disease progresses in stages, beginning with simple fat accumulation in liver cells and potentially advancing to more serious conditions:
- Simple Fatty Liver (Steatosis): The liver contains excess fat, but there is no significant inflammation or damage.
- Non-Alcoholic Steatohepatitis (NASH): Inflammation and liver cell damage occur, which can lead to fibrosis (scarring) of the liver.
- Cirrhosis: Advanced scarring of the liver impairs its function, leading to liver failure.
- Liver Cancer: In some cases, cirrhosis can progress to liver cancer.
Treatment and Management of Fatty Liver Disease
There is currently no specific medication approved to treat fatty liver disease, but management focuses on addressing the underlying risk factors and preventing further liver damage. The primary treatments include:
1. Lifestyle Modifications:
- Weight Loss: Gradual weight loss through diet and exercise is the most effective way to reduce fat in the Even a modest weight loss of 5-10% can improve liver health.
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats (such as those from fish, nuts, and olive oil) is Reducing the intake of processed foods, sugars, and trans fats can help prevent fatty liver progression.
- Exercise: Regular physical activity (at least 150 minutes of moderate exercise per week) helps manage weight, improve insulin sensitivity, and reduce fat in the liver.

2. Medications:
- While there are no specific drugs for fatty liver disease, some medications may be prescribed to manage related conditions, such as high cholesterol, high blood sugar, or hypertension. For example, statins can help lower cholesterol, while metformin can improve insulin resistance in people with diabetes.
- In the case of NASH (a more severe form of NAFLD), some medications, like pioglitazone (a medication used for diabetes), may be considered to reduce liver inflammation.
- For AFLD, the most effective treatment is to reduce or eliminate alcohol intake. In severe cases of liver damage, a liver transplant may be required.

3. Management of Co-existing Conditions:
- Diabetes management: Proper control of blood sugar through medication and lifestyle changes is essential for preventing fatty liver from worsening.
- Cholesterol and blood pressure control: Medications may be prescribed to manage cholesterol and blood pressure levels, further reducing the risk of liver damage.

- Regular Monitoring: People diagnosed with fatty liver disease should undergo regular monitoring through blood tests and imaging (such as ultrasound or MRI) to assess liver function and detect any progression toward cirrhosis or liver failure.

Preventing Fatty Liver Disease
Prevention of fatty liver disease revolves around maintaining a healthy lifestyle. The key steps include:
- Maintaining a healthy weight: Regular exercise and balanced nutrition are the cornerstones of weight management.
- Limiting alcohol consumption: Reducing or eliminating alcohol intake can significantly lower the risk of developing AFLD.

- Eating a healthy diet: A diet high in fiber, fruits, vegetables, and lean proteins can promote liver health.

- Managing chronic conditions: Keeping diabetes, high blood pressure, and cholesterol in check can reduce the likelihood of developing fatty liver disease.

Table of Low Glycemic Index Foods
| Food | Glycemic Index (GI) |
| Non-starchy vegetables (e.g., spinach, kale) | 0-15 |
| Whole grains (e.g., quinoa, barley) | 30-50 |
| Legumes (e.g., lentils, chickpeas) | 25-35 |
| Fruits (e.g., apples, pears, berries) | 30-50 |
| Nuts (e.g., almonds, walnuts) | 0-15 |
| Sweet potatoes | 44-61 |
| Oats (steel-cut) | 50-55 |
| Low-fat dairy (e.g., milk, yogurt) | 30-40 |
| Fish (e.g., salmon, trout) | 0-15 |
Incorporating foods with a low glycemic index helps manage blood sugar levels, a key factor in preventing or managing fatty liver disease.
Conclusion:
Fatty liver disease is a common yet often overlooked condition that can lead to severe liver damage if not managed properly. Early diagnosis and lifestyle changes are crucial for preventing progression to more serious liver disorders. While there is no single medication to cure fatty liver disease, managing contributing factors like obesity, diabetes, and alcohol consumption can significantly improve outcomes and liver function. Regular medical check-ups and a commitment to a healthier lifestyle are essential in managing and preventing fatty liver disease.




