Gastrointestinal Bleeding: Causes, Symptoms, and Diagnosis

Gastrointestinal bleeding, often referred to as GI bleeding, is a medical condition characterized by bleeding in the digestive tract. This can range from minor, hardly noticeable blood loss to severe, life-threatening hemorrhage. Understanding the causes, recognizing the symptoms, and obtaining a prompt diagnosis are crucial steps in managing GI bleeding effectively. In this blog post, we will delve into the key aspects of gastrointestinal bleeding to help you gain a better understanding of this condition.
Causes of Gastrointestinal Bleeding
GI bleeding can be caused by a variety of factors, which can broadly be categorized into upper and lower GI bleeding.
1.Upper GI Bleeding:
This type of bleeding originates from the upper part of the digestive tract, which includes the esophagus, stomach, and the first part of the small intestine (duodenum). Common causes of upper GI bleeding include:
- Peptic ulcers: Sores that develop on the lining of the stomach or the duodenum.
- Esophageal varices: Swollen blood vessels in the esophagus, often seen in individuals with liver disease.
- Gastritis: Inflammation of the stomach lining.
- Gastroesophageal reflux disease (GERD): Chronic acid reflux that can damage the esophagus.
- Mallory-Weiss tears: Tears in the esophagus or stomach lining, often caused by severe vomiting.
2.Lower GI Bleeding:
This type of bleeding originates from the lower part of the digestive tract, which includes the colon (large intestine) and rectum. Common causes of lower GI bleeding include:
- Diverticulosis: Small pouches forming in the colon wall that can bleed or become infected.
- Colorectal polyps: Non-cancerous growths in the colon that can bleed and, in some cases, become cancerous.
- Inflammatory bowel disease (IBD): Conditions like Crohn’s disease and ulcerative colitis can cause inflammation and bleeding in the intestines.
- Hemorrhoids: Swollen blood vessels in the rectum or anus that can bleed during bowel movements.
- Colorectal cancer: Cancerous growths in the colon or rectum can lead to bleeding.
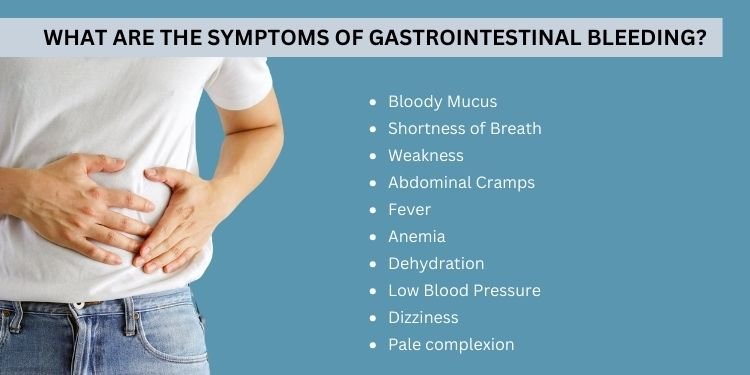
Symptoms of Gastrointestinal Bleeding
Recognizing the symptoms of GI bleeding is crucial for early intervention. Common signs and symptoms may include:
Blood in Stool:
This can appear as bright red blood in the stool or make the stool appear black and tarry.
Vomiting Blood:
If the bleeding is severe, it may result in vomiting blood or a substance that looks like coffee grounds.
Abdominal Pain:
Cramping or abdominal discomfort may occur.
Weakness and Fatigue:
Significant blood loss can lead to anemia, causing weakness and fatigue.
Dizziness or Fainting:
Low blood pressure due to bleeding may lead to dizziness or fainting.
Diagnosing Gastrointestinal Bleeding
Proper diagnosis of GI bleeding involves various tests and procedures, including:
- Endoscopy: Using a flexible tube with a camera, a healthcare provider can directly examine the upper or lower digestive tract to identify the source of bleeding.
- Imaging: X-rays, CT scans, or angiography may be used to visualize the digestive tract and locate the bleeding site.
- Blood Tests: Blood tests can reveal anemia and help determine the severity of bleeding.
- Stool Tests: Analysis of stool samples can detect the presence of blood.
- Capsule Endoscopy: A small, swallowable camera capsule can capture images of the entire digestive tract.
Conclusion
Gastrointestinal bleeding can be a concerning and potentially life-threatening condition. Identifying the underlying cause through proper diagnosis is essential for effective treatment. If you or someone you know experiences symptoms of GI bleeding, seek immediate medical attention. Early intervention can make a significant difference in the outcome and overall well-being of individuals affected by this condition.