What is Upper GI Endoscopy?
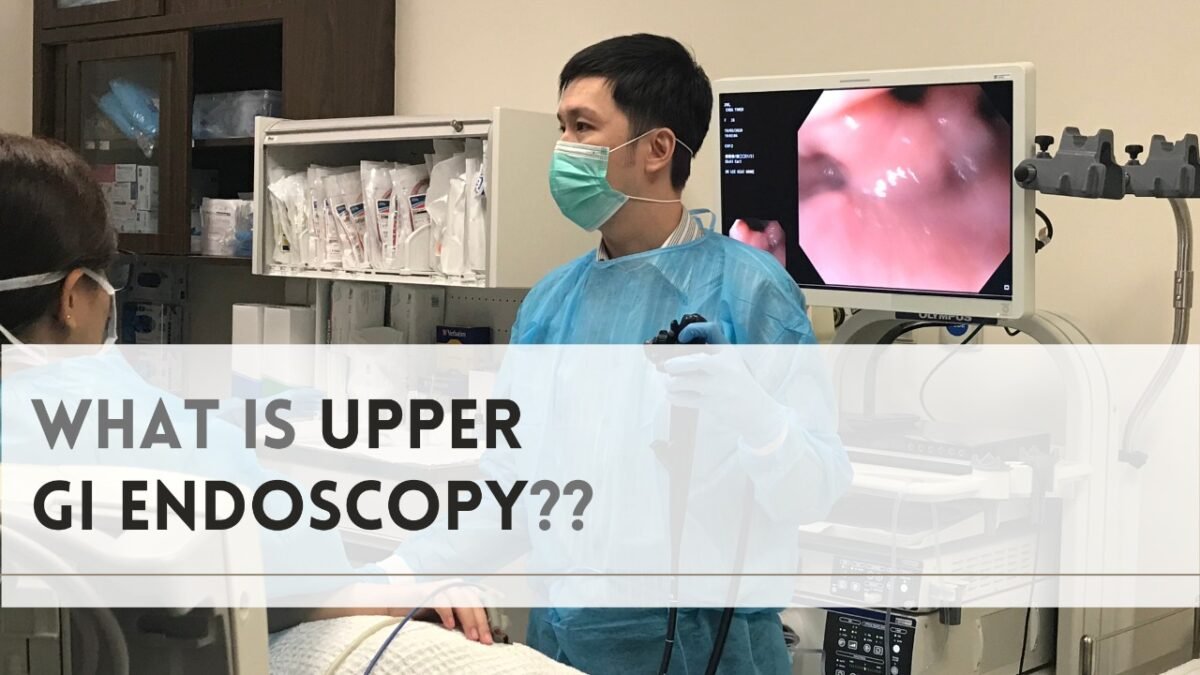
Upper GI endoscopy is a process in which a doctor examines the lining of your upper GI tract with an endoscope, which is a flexible tube with a camera. The treatment is performed by a gastroenterologist, surgeon, or other skilled health care expert, most typically with minimal sedation to help you relax.
An upper endoscopy is a technique that uses a tiny camera at the end of a long, flexible tube to visually examine your upper digestive tract. An endoscopy is used by a gastroenterologist (a specialist in digestive illnesses) to diagnose and, in some cases, treat conditions that affect the oesophagus, stomach, and first part of the small intestine (duodenum). Esophagogastroduodenoscopy is the medical word for an upper endoscopy. Upper endoscopies can be performed in a doctor’s office, an outpatient surgery centre, or a hospital.
Doctors perform upper GI endoscopy for a variety of reasons –
An upper endoscopy is a procedure that is used to diagnose and, in some cases, treat disorders that affect the upper part of your digestive systems, such as the oesophagus, stomach, and small intestine (duodenum).
An endoscopic procedure may be recommended by your doctor to:
- Investigate symptoms – An endoscopy can help your doctor figure out what’s causing digestive symptoms like nausea, vomiting, abdominal pain, swallowing problems, and gastrointestinal bleeding.
- Diagnose – An endoscopy may be used to obtain tissue samples (biopsy) in order to screen for diseases and symptoms including anaemia, bleeding, inflammation, diarrhoea, or digestive malignancies.
- Treat – Your gastroenterology doctor can use the endoscope to treat issues with your digestive system, such as stopping bleeding by burning a bleeding vessel, enlarging a narrow oesophagus, clipping off a polyp, or removing a foreign object.
Endoscopies are frequently coupled with other procedures, such as ultrasounds. To obtain specialised images of the wall of your oesophagus or stomach, an ultrasound probe may be added to the endoscope. Your doctor may use endoscopic ultrasound to create images of hard-to-reach organs like your pancreatic. High-definition video is used in newer endoscopes to produce crisper views.
Many endoscopes allow your doctor to employ narrow-band imaging, a technique that uses a special light to help detect precancerous disorders like Barrett’s oesophagus.
Risks Involved –
An endoscopy is a procedure that is quite safe. The following are examples of uncommon complications:
- Bleeding – If the process involves taking a piece of tissue for testing (biopsy) or treating a digestive system disease, your risk of bleeding issues following an endoscopy is higher. Such bleeding may necessitate a blood transfusion in rare situations.
- Infection – The majority of endoscopies consist of a visual examination and a biopsy, with a low risk of infection. When additional procedures are performed as part of your endoscopy, the risk of infection increases. Antibiotics can be used to treat the majority of illnesses. If you are at a higher risk of infection, your doctor may prescribe antibiotics before your procedure.
- The gastrointestinal tract is torn apart – If you have a tear in your oesophagus or another section of your upper digestive tract, you may need to be admitted to the hospital and have surgery to repair it. This complication is extremely rare, occurring in about one out of every 2,500 to 11,000 diagnostic upper endoscopies. Additional treatments, such as esophageal dilation to expand your oesophagus, enhance the risk.
By carefully following your doctor’s recommendations for preparation for an endoscopy, such as fasting and quitting certain medications, you can lower your chance of problems.
How do you get ready?
To prepare for your endoscopy, your doctor will give you precise instructions. Your doctor may ask you to
- Stop taking certain medications in some instances – In the days leading up to your endoscopy, you’ll need to cease using certain blood-thinning drugs. If certain procedures are performed during the endoscopy, blood thinners may increase your risk of bleeding. Your doctor will give you particular prescription instructions if you have chronic diseases such as diabetes, heart disease, or high blood pressure.
- Before the endoscopy, you should fast – To ensure your stomach is empty for the procedure, you must cease drinking and eating four to eight hours before your endoscopy.
- Make arrangements for a trip home – You can’t drive for 24 hours following the surgery for safety concerns, as the sedatives used during the procedure take time to wear off. You’ll need to arrange for transportation home after the treatment.
Before your endoscopy, tell your doctor about all the medications and supplements you’re using.
What you may anticipate
An endoscopy is a procedure that is used to examine the inside of the body. You’ll be asked to lie down on your back or side on a table for an upper endoscopy treatment. As the procedure progresses, keep the following in mind:
- Monitors are frequently worn on the body – Your health care team will be able to monitor your respiration, blood pressure, and heart rate as a result of this.
- A sedative may be administered to you – This medicine relaxes you throughout the endoscopy and is administered through a vein in your forearm.
- An anaesthetic may be sprayed into your mouth by your doctor – This drug will numb your throat in preparation for the long, flexible tube to be inserted (endoscope). To keep your mouth open, you may be requested to wear a plastic mouthguard.
- The endoscope will then be put into your mouth – As the scope travels down your throat, your doctor may urge you to swallow. There may be some discomfort in your throat, but it should not be painful.
You won’t be able to speak after the endoscope has passed down your throat, but you will be able to make noises. Your respiration is unaffected by the endoscope.
The endoscope is carefully retracted via your mouth after your doctor has finished the exam. Depending on your circumstances, an endoscopy can take anywhere from 15 to 30 minutes. After your endoscopy, you’ll be taken to a recovery area where you can sit or rest quietly. You are welcome to stay for an hour or so. This permits your doctor to keep an eye on you when the medication wears off.
Your situation will determine when you receive your endoscopic results. If your doctor performed an endoscopy to look for an ulcer, for example, you may get the results shortly after the surgery. You may have to wait a few days for results from the testing laboratory if he or she took a tissue sample (biopsy). Inquire with your doctor about when your endoscopic findings will be available.
Conclusion
For the initial investigation of individuals with dysphagia, upper GI endoscopy is an effective and suitable method. It improves early diagnosis and hence aids in the early commencement of acute abdominal treatment, which includes both pharmacological and surgical treatment.
If you were given a sedative, you should be able to wake up in around 2 hours, depending on the amount of sedative you were given. For a few hours, you may feel bloated, but this will pass. Unless otherwise instructed, you should be able to return to work the next day. The medical staff will inform you of what was discovered during the operation and discuss any necessary therapy or follow-up with you. Exercise on a regular basis should help your long-term health. Before you begin exercising, seek counsel from your healthcare provider or your primary care physician. An upper GI endoscopy and colonoscopy are usually safe and effective ways to determine if you have a digestive system disease.
For More Information visit Alfa Gastro & Liver Care Hospital.
